Understanding what capillary blood refers to is important because the glucometer provided by Tula measures your capillary glucose levels. Most glucometers are designed to measure capillary blood. If you have used a continuous glucose monitor (CGM) in the past, or are using one currently, don’t worry if your values differ slightly. Continuous glucose monitors measure glucose in the interstitial fluid of your body. While they are great for estimating whether blood sugar is going up or down and watching for trends, capillary blood glucose checks offer a more accurate representation of your true blood glucose level. Our glucometer is a fantastic tool that helps you see how health and lifestyle choices affect your body. It’s a great way to understand the impact that what you do and what you eat has on your blood glucose levels every day.
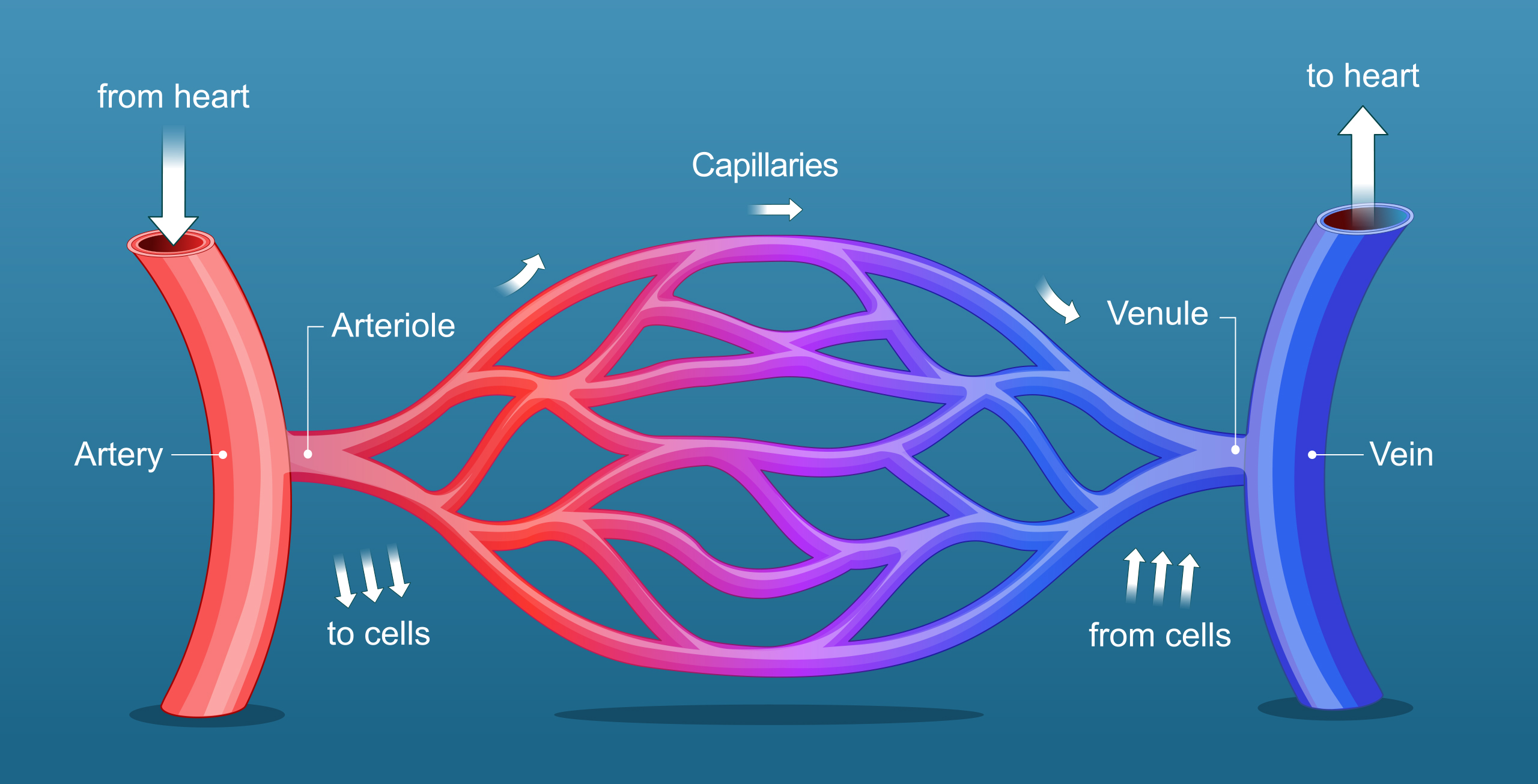
Capillary blood is used because it closely reflects the glucose levels in the body and is easily accessible. Capillary blood is the blood that flows through the smallest blood vessels in your body—think of where the blood flows into your fingertips. These vessels connect your arteries and veins together, which help transport oxygen and nutrients to your cells and remove waste products. Capillary blood glucose (CBG) refers to the sugar level circulating in your blood, which is measured from a small sample taken from a capillary, usually through a finger prick. This method provides a snapshot of your blood sugar at a specific moment.
Why Glucose Checks
Capillary blood glucose readings serve as your personal health dashboard. These quick checks provide real-time insights into your blood sugar levels, helping you make informed decisions about nutrition, movement, and medication. Regular monitoring helps you avoid dangerous highs and lows, keeps you feeling better, and offers essential data for your healthcare provider to tailor your treatment plan. Embrace these readings to help manage diabetes and enhance your overall well-being.
How to Check Capillary Blood Glucose (CBG) Levels
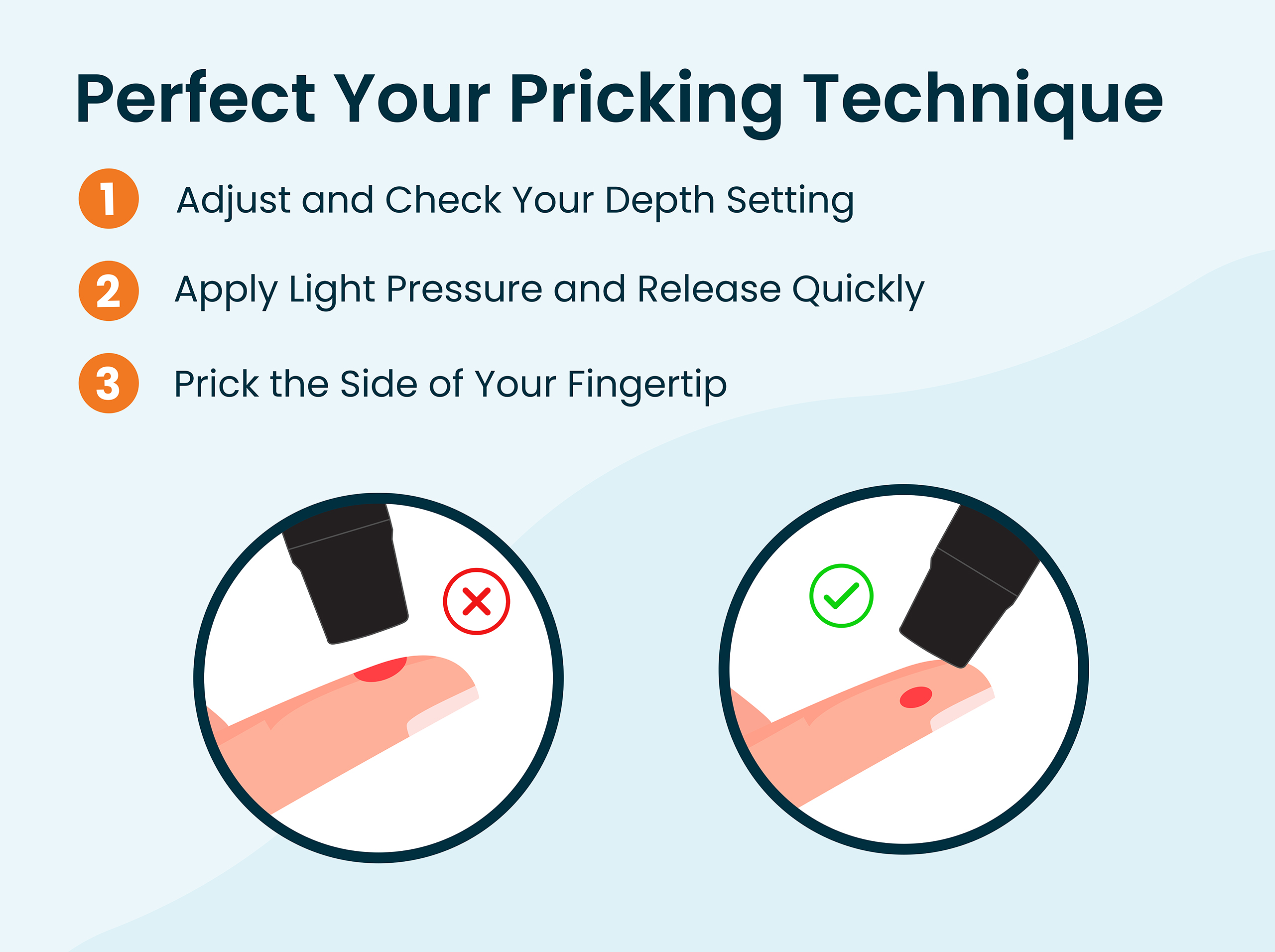
To check your capillary blood glucose levels, start by thoroughly washing your hands to ensure an accurate reading. Prepare your glucose meter and a test strip. Use a lancet to prick the side of your fingertip, as this area tends to be less painful. Gently squeeze your finger to obtain a small drop of blood and apply it to the test strip. Insert the strip into the meter, and within seconds, you’ll have your blood glucose reading. Documenting your readings over time can help you track blood glucose trends. When your glucometer syncs with the myTula app, you can review all your recorded blood sugar readings in one place.
Factors Affecting Accuracy
Technique: Improper technique, such as not cleaning the finger properly or squeezing it too hard, can affect the accuracy of your blood glucose reading. Squeezing can dilute the blood sample with tissue fluid, and it increases the probability of hemolysis—the breaking of red blood cells. Hemolysis can lower the concentration of plasma glucose (11).
Clean the Finger: Wash hands or use an alcohol wipe to clean your finger(s) and let them dry before the finger poke. Even when cleaning your finger beforehand, the first drop of capillary blood should be discarded, and the second drop of blood should be used for sampling (5). The first blood drop can contain interstitial and intracellular fluid that may contaminate the sample (4). Discarding the first drop also ensures that no residue from the alcohol wipe contaminates the blood drop.
Blood Sample Size: Not applying enough blood to the test strip can cause an error or an inaccurate reading. Make sure to use a generous drop of blood. Be aware that some point-of-care devices require the first drop of blood, so it may vary depending on the glucometer.
Test Strip Issues: Expired blood glucose test strips can impact accuracy because the enzymes on the strips, which react with glucose to produce a reading, degrade or break down over time. Extreme temperatures and humidity can also impact the chemistry of the test strips.
Hematocrit Levels: Changes in the amount of red blood cells can impact readings. To know if your hematocrit levels are too high or low, you typically need a blood test. Low hematocrit (anemia) may cause your readings to show higher blood glucose results, while high hematocrit may cause lower readings (7). Your hematocrit levels can be checked through a blood test during your doctor’s appointment, either from a blood draw or using a drop of blood from your fingertip analyzed by a smaller device.
Remember, capillary blood glucose measurements are like a snapshot in time; they don’t provide the whole picture. This is why it’s essential to pay attention to what you do before and after your readings to identify patterns that impact your blood sugar. Rather than focusing solely on individual readings, tracking trends over time will help you understand what is working in managing your diabetes. If you’re unsatisfied with your numbers, consider discussing potential experiments with your HealthCoach to help bring about positive changes in your blood glucose levels.
Sending Health Your Way!
The Tula Clinical Team
Austin MS, RDN, CSR, LDN, CD
Aubree RN, BSN
Tula Takeaways |
|---|
| 1. Importance of Capillary Blood Glucose Checks: Capillary blood glucose readings provide an immediate snapshot of your blood sugar levels at a specific moment. |
| 2. Factors Affecting Accuracy: Several factors can impact the accuracy of your readings, such as improper technique, insufficient blood sample size, expired test strips, and changes in hematocrit levels. Being mindful of these can help you obtain more reliable results and better manage your diabetes. |
| 3. Know Your Baseline: Regularly testing your blood sugar levels will help you establish your baseline. This serves as a great starting point for managing your blood sugar effectively. |
The LIVE TULA blog is informational and not medical advice. Always consult your doctor for health concerns. LIVE TULA doesn’t endorse specific tests, products, or procedures. Use the information at your own risk and check the last update date. Consult your healthcare provider for personalized advice.






