Article Quick Links
Part 1: The Hidden Dangers of Microvascular Complications >
Part 2: Protecting Yourself: Preventing Microvascular Damage >
Part 3: Macrovascular Complications: The Large Vessel Concerns >
Part 4: Macrovascular Prevention and Treatment: Taking Control >
Part 1: The Hidden Dangers of Microvascular Complications
In Part 1, let’s explore the hidden dangers of microvascular complications.
Microvascular complications refer to damage in the body’s small blood vessels and are often the first warning signs of more serious diabetes-related issues. These complications can impact essential organs like the eyes, kidneys, and nerves and are early indicators that diabetes management needs attention. Left unchecked, they can progress to severe outcomes such as nerve damage, vision loss, or kidney disease. Understanding and addressing microvascular complications early is crucial for preventing long-term health problems and maintaining overall well-being.
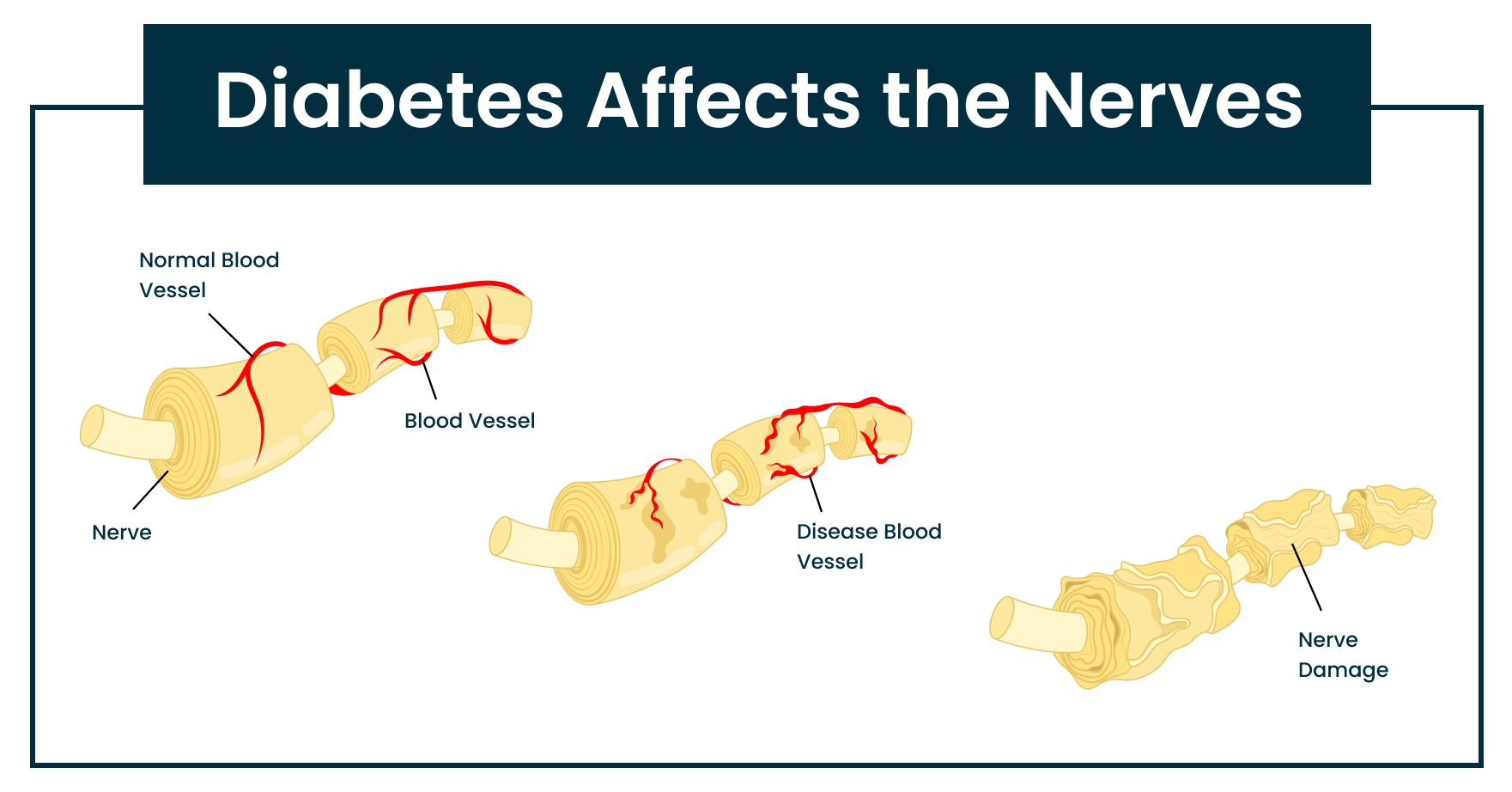
Neuropathy: The Nerve Damage Dilemma
High blood sugar can lead to diabetic peripheral neuropathy, a condition where nerve damage causes symptoms like numbness, tingling, pain, and muscle weakness, mostly in the legs and feet. Prevention through effective blood sugar control is essential, as treatments are limited once significant nerve damage occurs. According to the American Diabetes Association, keeping blood sugar levels within target ranges can dramatically reduce the risk of neuropathy. Early detection and management can slow the progression of nerve damage and improve quality of life.
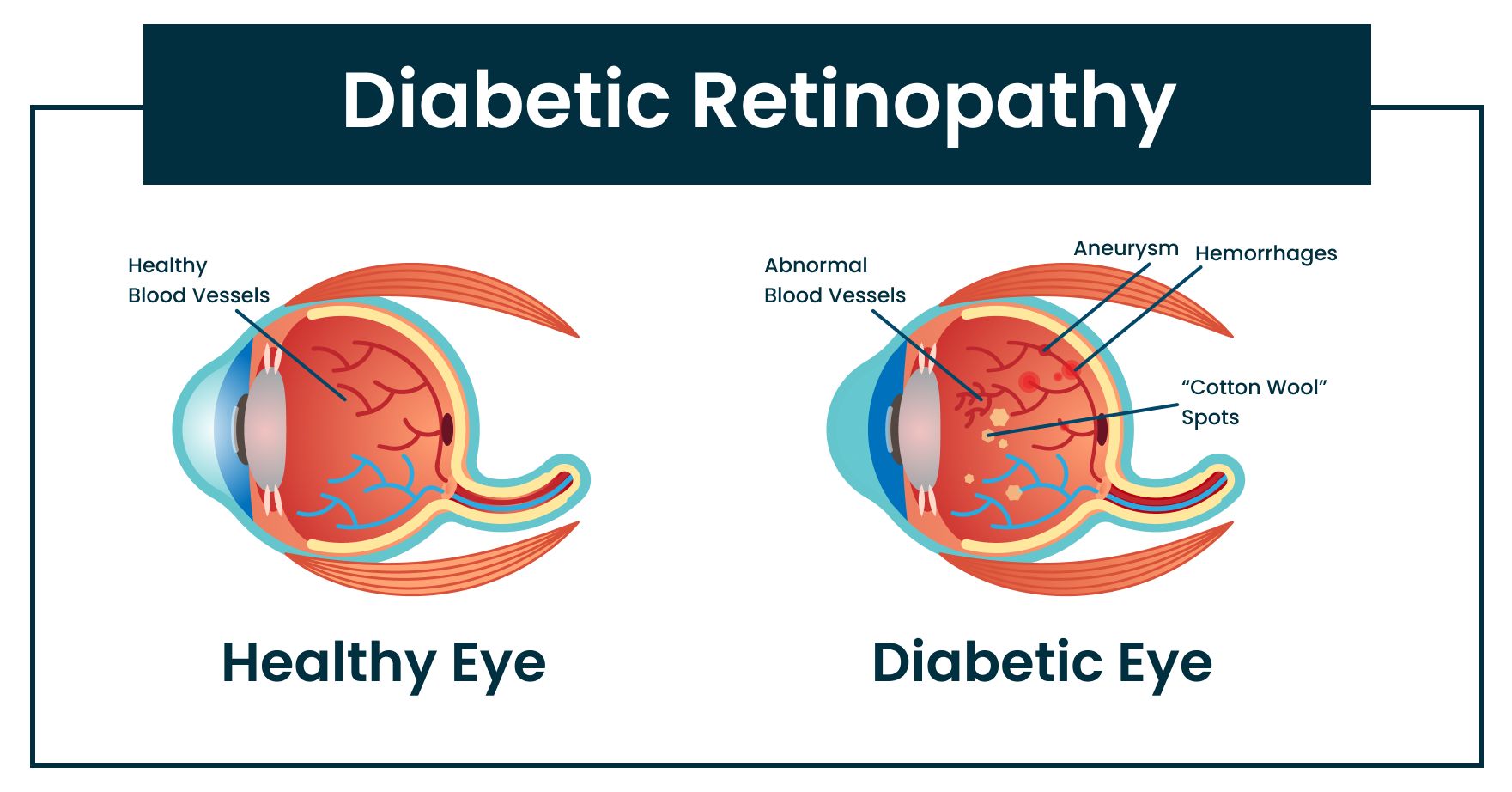
Diabetic Retinopathy: Protecting Your Vision
Diabetic retinopathy is a leading cause of preventable vision loss (29), occurring when high blood sugar damages the small blood vessels in the retina, leading to visual changes. Regular eye exams are crucial for early detection, and managing blood glucose and blood pressure levels can help prevent or delay the condition. Early intervention greatly improves quality of life, so be sure to discuss your treatment plan with your healthcare provider and Tula Nurse to address factors that may affect your care.
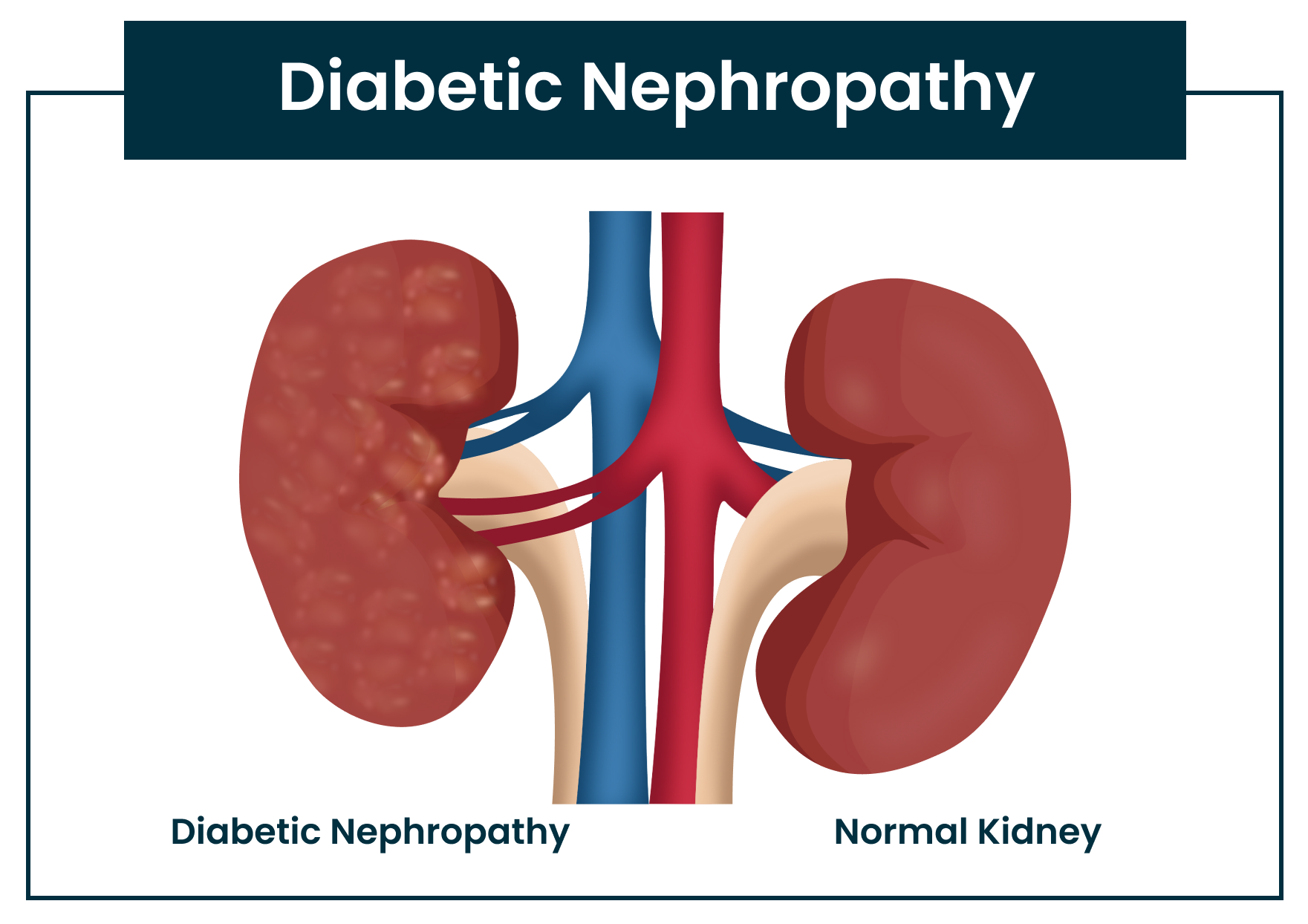
Nephropathy: Kidney Function at Risk
Nephropathy refers to the decline in kidney function, which impacts the kidneys’ ability to filter waste, regulate blood pressure, produce red blood cells, and synthesize certain hormones, such as the active form of vitamin D. This decline can start before a formal diagnosis of kidney disease. Early detection through regular blood and urine tests is key to slowing its progression. Check out the blog “Cracking the Code: How Blood Pressure and Lab Tests Reveal Your Kidney Health” for more details on your lab results. Improving kidney health can be as simple as increasing water intake, reducing protein consumption, adding more fruits and vegetables to your diet, losing excess weight, and working with your healthcare provider to manage blood pressure (12). These strategies have been shown to slow or even improve kidney function in those with diabetes (11).
Part 2: Protecting Yourself: Preventing Microvascular Damage
In Part 1, we uncovered the hidden dangers of microvascular complications. Now, in Part 2, we’ll explore practical tips and strategies to help protect yourself and prevent further microvascular damage.
Maintaining stable blood sugar levels is the most critical step in preventing and managing complications like nephropathy, retinopathy, and neuropathy. Experts recommend targeting an A1C of less than 7% for people with diabetes to reduce the risk of these serious health conditions.
But what if these complications already exist? While advanced complications may not be reversible, there is hope in preventing further damage. A combination of lifestyle changes, nutritional adjustments, supplements, and medications can help manage symptoms and slow their progression. Always consult your healthcare provider before making any changes to your treatment plan, including starting or stopping supplements or medications.
Benefits of Alpha-Lipoic Acid in Prevention
Alpha-lipoic acid (ALA) is a potent antioxidant that can help alleviate the symptoms of neuropathy, particularly diabetic neuropathy. Fluctuating blood sugar levels contribute to oxidative stress, which damages nerve cells. ALA helps reduce this damage by decreasing oxidative stress and improving blood flow and nerve signaling, which may relieve symptoms such as pain, burning, and numbness. Studies indicate that administering ALA intravenously at 600 mg per day for three weeks can significantly reduce neuropathy symptoms. Oral doses of ALA, ranging from 600 to 1,800 mg per day, are also beneficial, though slightly less effective than IV administration (16, 17). Anyone considering ALA should consult with a healthcare provider to determine the appropriate dosage and ensure it does not interfere with other medications or health conditions.
How B Vitamins Can Help With Microvascular Protection
B vitamins, including B1, B6, and B12, play a crucial role in maintaining healthy nerve function. A deficiency in these vitamins can lead to nerve function problems, which is particularly common in people with diabetes. This is because diabetes can cause the body to deplete B vitamins more quickly and absorb them less effectively, resulting in deficiencies.
For example, insufficient levels of vitamin B12 can lead to nerve damage, potentially worsening diabetic neuropathy. Supplementing with these B vitamins can help improve nerve health by ensuring that the nerves receive the necessary nutrients for proper function (18).
Take note! It’s essential to consult a healthcare provider about checking vitamin B12 levels. Additionally, discussing your current intake with a dietitian can help determine if you are not meeting your daily needs for other B vitamins. Understanding these levels and intakes may lead to the recommendation of supplements, which can help prevent or treat nerve damage.
The Role of N-Acetyl Cysteine in Managing Complications
Another supplement to consider is N-acetyl cysteine (NAC). NAC is a synthetic form of the amino acid cysteine, which is a building block for proteins. Cysteine is then utilized to produce glutathione—a powerful antioxidant naturally generated by the liver that protects the brain and eyes. While oral glutathione supplements are available, they tend to be more expensive and less effective because they often break down before being absorbed by the body. NAC is converted into cysteine in the body, supporting glutathione production. Although cysteine can be found in foods such as garlic, sunflower seeds, and onions, NAC supplements provide higher concentrations that may be more effective.
In cases of diabetic retinopathy, a common eye problem in people with diabetes, oxidative stress and inflammation are significant concerns. NAC helps increase glutathione levels, reducing oxidative stress and inflammation, thereby protecting the retina.
Consult your healthcare provider or dietitian about NAC and its potential to improve your eye health, particularly in slowing down diabetic retinopathy by combating oxidative stress and inflammation.
How a Low-Protein Diet Can Benefit Kidney Function
Scientists have discovered that reducing protein intake can benefit individuals with kidney problems. Research recommends a specialized diet called the “Plant-Dominant Low Protein Diet” (PLADO). On this diet, you should consume 0.6 to 0.8 grams of protein for each kilogram of your body weight each day (30). At least half of this protein should come from plant sources, such as beans, nuts, and grains.
Protein can be detrimental to the kidneys because it produces waste products that they must filter out. A high protein intake forces the kidneys to work harder, potentially worsening kidney disease. Reducing protein intake decreases the amount of waste that the kidneys need to process.
For example, if you weigh 50 kilograms (approximately 110 pounds), you should aim to consume between 30 and 40 grams of protein each day. It’s also crucial to prioritize whole, unprocessed foods and keep your sodium intake below 3 grams per day. Additionally, you should strive to consume 25 to 30 grams of fiber daily, which can be obtained from fruits, vegetables, and whole grains.
Here are some tips for following the PLADO diet:
- Eat more plant-based proteins like beans, lentils, tofu, and quinoa.
- Avoid processed foods and meats that contain added phosphorus or potassium.
- Choose whole fruits and vegetables over juices and processed snacks.
- Ensure you get enough calories from healthy sources like whole grains, fruits, and vegetables to maintain your energy levels.
- Ask your doctor to check your vitamin B12 levels, especially if you are primarily consuming plant-based foods.
Part 3: Macrovascular Complications: The Large Vessel Concerns
In Part 1, we uncovered the hidden dangers of microvascular complications. In Part 2, we provided practical tips and strategies to help protect yourself and prevent further microvascular damage. Now, in Part 3, we’ll explore the large vessel concerns of macrovascular complications.
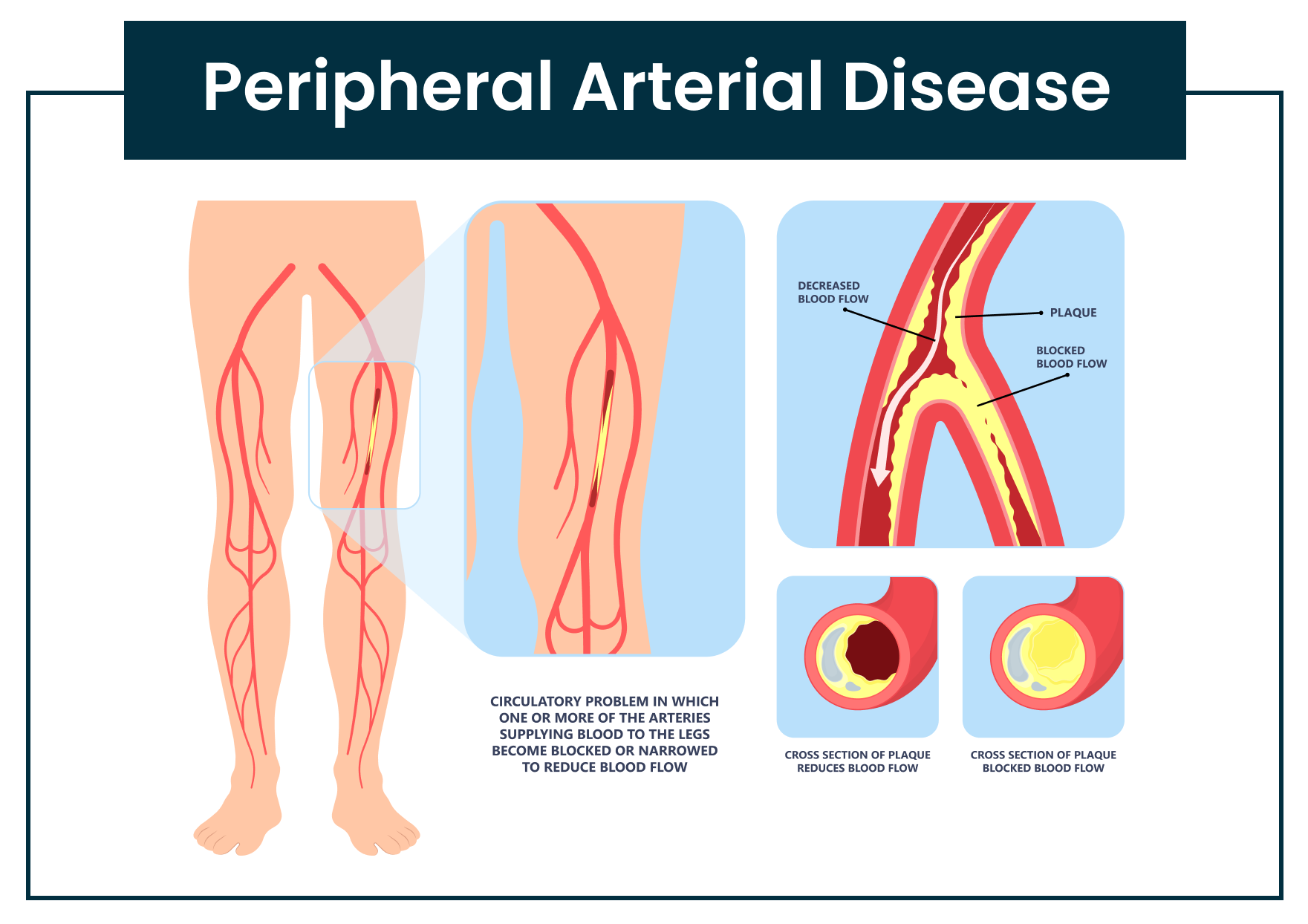
We’ve reviewed microvascular issues; now let’s move on to macrovascular complications. “Macro” means “large,” so these complications affect the larger blood vessels. The two most common macrovascular complications are peripheral arterial disease (PAD) and coronary heart disease (CHD). It is crucial to prevent or closely manage these conditions if they occur, as they are major risk factors for life-threatening outcomes (23).
Peripheral Arterial Disease (PAD): When Blood Flow Slows
Peripheral Arterial Disease (PAD) occurs when arteries narrow, reducing blood flow to the limbs. This can cause symptoms such as fatigue and discomfort and, in severe cases, may lead to amputation. The good news is that lifestyle changes—such as improving nutrition, increasing body movement, and managing weight—can effectively help manage PAD. It’s important to watch for symptoms like swelling or pain, as early treatment can make a significant difference. According to the American Heart Association, individuals with diabetes are at a higher risk for PAD because elevated blood sugar levels can damage large blood vessels. On a positive note, studies show that supervised exercise programs can significantly improve walking distance and reduce symptoms in PAD patients (27).
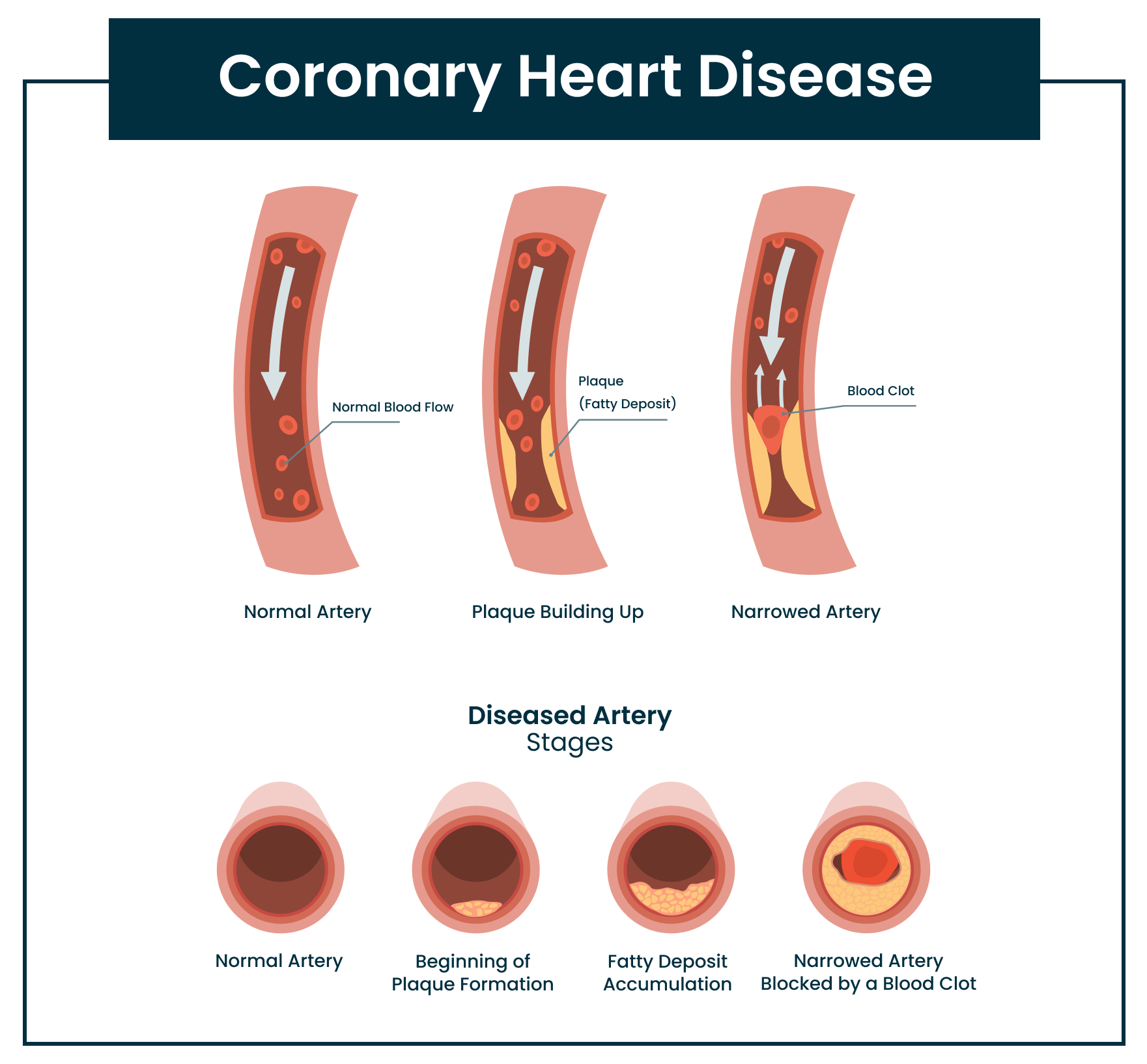
Coronary Heart Disease (CHD): The Heart of the Matter
When blood vessels are damaged by high blood sugar, it can harm the inner lining of the arteries. In response, the body may produce extra cholesterol to repair this damage; however, over time, this cholesterol builds up and forms plaque. This plaque narrows and hardens the arteries, leading to coronary heart disease (CHD). CHD can result in reduced blood supply to the heart or slow blood flow enough to increase the risk of clotting, both of which can trigger heart attacks. Managing blood sugar, knowing your cholesterol levels, monitoring blood pressure, and discussing risks with your health provider are crucial steps to preventing CHD. The American College of Cardiology emphasizes that diabetes doubles the risk of CHD, making diligent blood glucose management essential. Research shows that lifestyle modifications, such as proper nutrition and regular physical activity, can reduce CHD incidence by up to 50% in high-risk individuals (28).
Part 4: Macrovascular Prevention and Treatment: Taking Control
In Part 1, we uncovered the hidden dangers of microvascular complications. In Part 2, we provided practical tips and strategies to help protect yourself and prevent further microvascular damage. In Part 3, we revealed the large vessel concerns of macrovascular complications. Now, in Part 4, we’ll explore macrovascular prevention and treatment.
Providing actionable advice for macrovascular prevention empowers individuals to take control of their health and reduce the risk of serious complications. By focusing on practical steps, like managing blood sugar, cholesterol, and blood pressure, we can help prevent conditions such as coronary heart disease and peripheral arterial disease.
Know Your Numbers
Monitoring your blood sugar, cholesterol (especially LDL), and blood pressure is key to reducing your risk of peripheral vascular disease and coronary heart disease. By understanding your baseline, you can focus on the areas that need improvement and take control of your health.
Incorporate Antioxidants
Incorporating antioxidant-rich foods into your diet can help protect large blood vessels. Foods such as berries, nuts, seeds, and dark leafy greens are excellent sources of antioxidants, and organic tart cherry juice concentrate is another great option to easily add potent antioxidants throughout your day. Recent studies support the cardiovascular benefits of antioxidants. For example, He et al., in the Journal of the American Heart Association, found that higher dietary antioxidant intake is linked to a reduced risk of coronary heart disease. Similarly, research by Cocate et al. published in Nutrients highlighted the positive effects of berries and nuts on blood vessel function and heart health. These findings emphasize the importance of antioxidant-rich diets in preventing macrovascular complications in individuals with diabetes (20, 21). Since oxidative stress occurs whenever blood sugar levels are elevated, these antioxidants play a crucial role in combating the oxidative damage caused by blood sugar fluctuations.
Include Omega-3 Fatty Acids
Omega-3 fatty acids are considered one of the “good” fats that should be regularly included in your diet. Research shows that consuming foods rich in omega-3s—such as chia seeds, flaxseeds, walnuts, tuna, and salmon—can help improve triglyceride levels, which contribute to total cholesterol. The Journal of the American College of Cardiology also highlights the benefits of omega-3 fatty acid supplements in lowering triglyceride levels and reducing the risk of heart disease (22). Although omega-3s don’t lower LDL, recent research shows that omega-3 supplementation reduces the risk of major cardiovascular events, heart attacks, and even death following a heart attack (31).
Explore if Red Yeast Rice Extract Is Good for You
Red yeast rice extract is derived from rice fermented with a specific type of yeast and contains a compound similar to the cholesterol-lowering drug lovastatin. This supplement may help reduce cholesterol, decrease inflammation, improve blood flow, and support overall heart health. Typically, individuals take between 600 mg and 1,200 mg daily, divided into two doses. However, it’s essential to consult your health provider before using red yeast rice, as it can cause side effects such as muscle pain and liver issues. It is not recommended for people with liver or kidney disease or those taking certain medications like antibiotics or antifungals (24, 26).
Increase Fiber Intake
Health providers often recommend increasing fiber intake, especially soluble fiber, when cholesterol levels are high, and for good reason! Soluble fiber can reduce cholesterol absorption in the bloodstream. One study even showed that higher dietary fiber intake is linked to a lower risk of heart disease. Fiber-rich foods include chia seeds, beans, lentils, oats, barley, apples, bananas, and berries. Unless otherwise directed by a gastroenterologist, everyone should aim for at least 28 grams of fiber daily (29).
Balance 3 Key Minerals: Sodium, Potassium, and Magnesium
Managing blood pressure is crucial since high blood pressure is a major risk factor for both coronary heart disease (CHD) and peripheral vascular disease (PVD). While taking prescribed blood pressure medications is important, dietary changes—such as ensuring adequate potassium and magnesium intake while avoiding excessive sodium—can lead to improved blood pressure control and potentially decrease the need for medication. Potassium helps manage sodium levels in the body and eases tension in large blood vessels. Magnesium also helps relax blood vessels and acts as an antioxidant, providing similar benefits as mentioned earlier. A great way to start balancing these minerals is by reading nutrition labels, limiting sodium intake to 3 grams per day, and incorporating foods rich in potassium and magnesium into your daily routine.
Potassium-Rich Foods:
- Avocado
- Bananas
- Beets
- Coconut Water
- Potatoes
- Spinach (Cooked)
- Sweet Potatoes
- Tomatoes
- White Beans
Magnesium-Rich Foods:
- Almonds
- Black Beans
- Chia Seeds
- Dark Chocolate (80-85% Dark)
- Pumpkin Seeds
- Quinoa
- Spinach
Sending Health Your Way!
The Tula Clinical Team
Austin MS, RDN, CSR, LDN, CD
Aubree RN, BSN
Tula Takeaways |
|---|
Part 1 |
| 1. Early Detection is Critical: Microvascular complications often serve as early warning signs for more severe health problems, such as nerve damage, vision loss, and kidney disease. Regular monitoring and early intervention are key to preventing long-term damage. |
| 2. Blood Sugar Control is Essential: Effective blood sugar management significantly reduces the risk of complications like neuropathy, retinopathy, and nephropathy. Keeping blood glucose within target ranges can slow the progression of nerve, eye, and kidney damage. |
| 3. Comprehensive Prevention: Beyond glucose control, regular eye exams, kidney function tests, and maintaining a healthy lifestyle—through hydration, balanced nutrition, and blood pressure management—are vital in preventing or slowing the progression of microvascular complications. |
Part 2 |
| 1. Maintain Stable Blood Sugar Levels: Keeping blood sugar levels stable is crucial for preventing complications like nephropathy, retinopathy, and neuropathy. Aim for an A1C of less than 7% to reduce the risk of these serious health conditions. |
| 2. Incorporate Key Supplements: Consider adding supplements such as Alpha-Lipoic Acid (ALA) and B vitamins to your regimen. ALA can help alleviate neuropathy symptoms by reducing oxidative stress, while B vitamins support healthy nerve function and can prevent nerve damage associated with deficiencies. |
| 3. Follow a Plant-Dominant Low Protein Diet (PLADO): Reducing protein intake can benefit kidney function, particularly for those with kidney problems. Aim for 0.6 to 0.8 grams of protein per kilogram of body weight daily, focusing on plant-based sources to minimize waste and support kidney health. |
Part 3 |
| 1. Manage PAD with Lifestyle Changes: Peripheral Arterial Disease (PAD) can reduce blood flow to your limbs, but making changes to your nutrition, exercise routine, and weight management can help significantly reduce symptoms and improve mobility. |
| 2. Prevent CHD by Controlling Blood Sugar: High blood sugar can lead to coronary heart disease (CHD) by damaging arteries and building up plaque. Managing your blood sugar, cholesterol, and blood pressure levels is key to reducing CHD risk. |
| 3. Diabetes Increases Risk for PAD and CHD: Diabetes doubles your risk for both PAD and CHD, so early detection and lifestyle modifications, like improving diet and increasing physical activity, are critical to preventing these life-threatening complications. |
Part 4 |
| 1. Know Your Numbers: Regularly monitor your blood sugar, cholesterol (especially LDL), and blood pressure. Understanding these key health metrics allows you to identify areas for improvement and empowers you to take control of your health. |
| 2. Incorporate Antioxidants and Omega-3s: Add antioxidant-rich foods like berries, nuts, and dark leafy greens, along with omega-3 fatty acids found in chia seeds, flaxseeds, and fatty fish. These nutrients help protect your cardiovascular system and reduce the risk of serious complications. |
| 3. Increase Fiber Intake: Focus on boosting your dietary fiber, especially soluble fiber, which can help lower cholesterol levels and improve heart health. Aim for at least 28 grams of fiber daily by including foods such as beans, lentils, oats, and fruits like apples and bananas. |
| 4. Balance Key Minerals: Maintain a healthy balance of sodium, potassium, and magnesium in your diet. Reducing sodium intake while increasing potassium and magnesium can enhance blood pressure control and support overall heart health. Incorporate potassium-rich foods like bananas and spinach, as well as magnesium-rich foods like almonds and dark chocolate. |
The LIVE TULA blog is informational and not medical advice. Always consult your doctor for health concerns. LIVE TULA doesn’t endorse specific tests, products, or procedures. Use the information at your own risk and check the last update date. Consult your healthcare provider for personalized advice.






