When it comes to maintaining good health, understanding the signals our bodies send is crucial. This is especially true for blood pressure and kidney function—two vital aspects of overall well-being. Let’s explore the key home monitoring and lab tests that provide valuable insights into these areas.
Systolic and Diastolic Blood Pressure
Blood pressure readings consist of two numbers: systolic and diastolic. The systolic number (the top number) measures the pressure in your arteries when your heart beats, while the diastolic number (the bottom number) measures the pressure when your heart rests. Think of a hose with a kink in it—water must push harder to get through the kink, increasing the pressure. This is similar to high blood pressure. Over time, combined with uncontrolled diabetes, this increased pressure can lead to kidney disease, making regular blood pressure monitoring essential.
For most people with diabetes, it is recommended to keep blood pressure below 130/80 mmHg, but your doctor may set a different target based on your individual health needs (Flack, 2020). It’s important to note that 130/80 mmHg is not necessarily optimal blood pressure for everyone. Discussing your specific target with your healthcare provider can help personalize your care while considering recommendations from the American Diabetes Association (ADA).
Kidney Disease
Your kidneys are two bean-shaped organs located just below your rib cage, toward your back. Though small, they are incredibly powerful—so much so that we cannot live without them (unless receiving life-saving dialysis treatments).
The kidneys play a crucial role in filtering toxins and metabolic waste from the blood, regulating blood pressure, maintaining fluid and acid-base balance, producing hormones (including an active form of vitamin D!), and keeping electrolyte levels in check. Given their essential functions, it’s clear how vital these organs are to overall health.
Unfortunately, diabetes and high blood pressure are the leading causes of kidney disease and kidney failure. This makes it especially important to monitor lab tests that provide insight into kidney health. Here are some key lab values to keep an eye on moving forward.
BUN: The Protein Processing Indicator
Blood urea nitrogen (BUN) is another important indicator of how well your kidneys are processing waste from protein breakdown. An elevated BUN (greater than 20 mg/dL) can result from various factors and serves as an early “red flag” for kidney health. High BUN levels may be caused by dehydration, excessive protein intake, or insufficient dialysis in individuals with kidney issues.
However, just like with creatinine, lower BUN levels (below 10 mg/dL) don’t always indicate better health. Low BUN levels may be associated with liver problems or poor nutritional intake.
If you have high BUN levels, here are some steps you can take:
- Drink Plenty of Water: Dehydration can raise BUN levels, so ensure you’re drinking enough fluids each day.
- Watch Your Protein Intake: Consuming too much protein can increase BUN levels. Follow a balanced diet and consult your doctor or dietitian to determine the right amount of protein for you.
- Check Your Medications: Certain medications can affect BUN levels. Your Tula RN can review your medications and help prepare you for a conversation with your doctor, who can assess whether any adjustments are needed.
- Ensure Proper Dialysis: If you’re on dialysis, consult your healthcare professional to confirm you’re receiving the correct amount. Skipping or shortening dialysis sessions can lead to elevated BUN levels.
- Schedule Regular Check-Ups: Routine visits to your healthcare provider can help monitor and manage your BUN levels effectively.
- Follow Treatment Plans: Always adhere to the treatment plans and guidance provided by your healthcare provider to support kidney health.
Creatinine: The Muscle Metabolism Marker
Creatinine is a waste product produced by your muscles. Normally, healthy kidneys filter creatinine out of your blood, keeping its levels within a normal range. To better understand creatinine, think of your blood as a river, your kidneys as a filter, and creatinine as dirt that needs to be removed. If your kidneys aren’t functioning properly, creatinine and other harmful substances build up in your blood, which can be dangerous.
Creatinine levels vary based on factors such as race and gender. While elevated creatinine can be an early warning sign of kidney issues, it does not necessarily indicate kidney disease. High creatinine levels often suggest reduced kidney function, which can also contribute to high blood pressure. Conversely, low creatinine levels may result from low muscle mass or inadequate nutrition, but they don’t always indicate better health. Monitoring creatinine levels is essential for assessing kidney function and maintaining stable blood pressure.
eGFR: Estimated Percent of Your Kidney Function
The estimated Glomerular Filtration Rate (eGFR) is a calculated measurement based on serum creatinine, age, sex, and other biometric factors. This measurement helps assess kidney function. If eGFR is low, additional testing, such as a urinalysis, is typically used to confirm a diagnosis of chronic kidney disease.
A normal eGFR is considered to be greater than 90, with no proteinuria (excess protein in the urine). To make it easier to understand, think of eGFR as an estimate of how efficiently your kidneys are filtering waste. For example, if your eGFR is 70, your kidneys are functioning at approximately 70% of their capacity. Lower eGFR levels indicate varying stages of kidney damage.
It’s important to remember that eGFR results (shown in this chart) should be interpreted alongside a urinalysis to check for protein levels in the urine. Be sure to discuss your results with your healthcare provider for a comprehensive assessment of your kidney health.
Potassium: The Electrolyte of Movement
Potassium levels are crucial indicators of kidney health. This essential mineral plays a vital role in muscle contractions, nerve function, and insulin regulation. An imbalance in potassium levels can have significant consequences.
High potassium levels (hyperkalemia), often caused by medications, constipation, or chronic illnesses, can lead to symptoms such as fatigue, muscle cramps, and heart palpitations, potentially increasing the risk of a heart attack. On the other hand, certain medications can cause potassium levels to drop too low (hypokalemia), which can also result in serious health complications.
Maintaining the proper potassium balance is essential, as both hyperkalemia and hypokalemia can indicate underlying issues with kidney function and overall health. Regular monitoring and medical guidance can help ensure potassium levels remain within a healthy range.
If you have elevated potassium levels, we recommend:
- Talking to your doctor about the medications you are taking. Even over-the-counter medications, such as pain relievers, should be discussed, as they can affect your potassium levels.
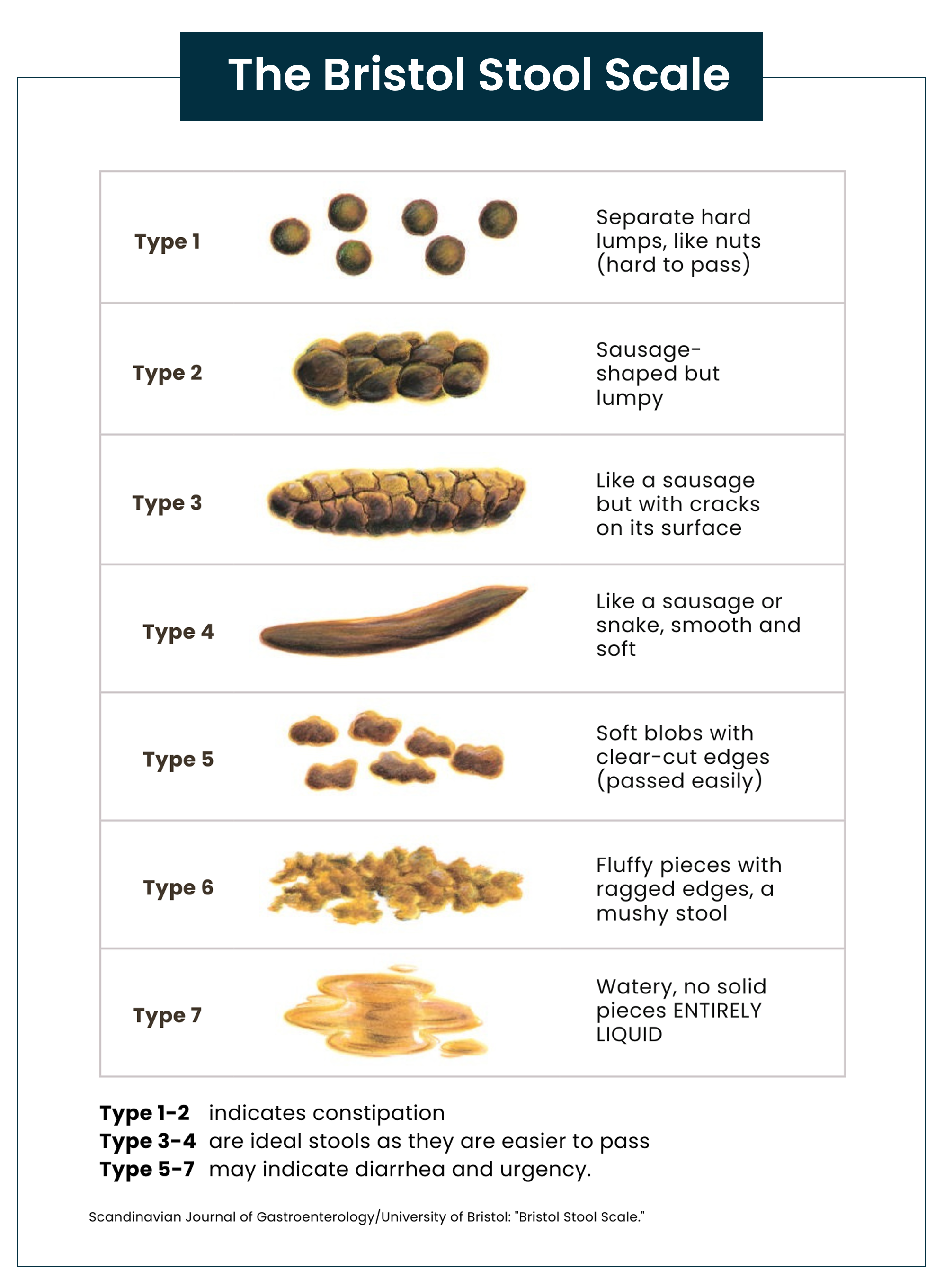
- Checking your bowel habits. If you are not having a daily bowel movement, this may contribute to elevated potassium levels. Increase your fiber intake to ensure you are passing “Type 3” or “Type 4” stool each day.
- Decrease your animal protein intake. Animal protein contains high levels of potassium. Unfortunately, low-potassium diets often focus only on reducing potassium-rich fruits and vegetables, but seafood, meat, poultry, and even Greek yogurt contain more potassium than many fruits and vegetables. Additionally, excessive consumption of animal-based proteins can lead to constipation, which, as mentioned, can contribute to elevated potassium levels.
- Be mindful of plant-based protein choices. While lentils are high in potassium and may need to be avoided, alternatives such as chickpeas, tofu, tempeh, two tablespoons of natural peanut butter, or black beans are excellent plant-based protein sources for individuals with late-stage kidney disease.
A key difference between plant-based and animal-based proteins for individuals who need to reduce potassium intake is that potassium from plant-based proteins is not absorbed in the same way as potassium from animal proteins. The dietary fiber in plant-based foods can hinder the absorption of excess potassium, while potassium from animal-based proteins is more readily absorbed into the bloodstream. This can contribute to an imbalance in nutrient intake for individuals managing potassium levels due to kidney conditions.
This distinction is important for those struggling with high potassium or who are on medications that elevate potassium levels. Unfortunately, there is often misinformation suggesting that individuals should decrease their intake of fruits and vegetables when potassium levels are high. It’s actually better to reduce animal protein consumption and continue benefiting from the fiber in plant-based proteins.
Important Note: Even for those without a kidney condition, animal-based proteins also carry a higher acid load for the body/kidneys, so this still isn’t a great way to get potassium for those who are looking to increase potassium intake.
Sodium: The Fluid Balance Regulator
Sodium is an essential electrolyte and mineral for cellular function and fluid balance. While there are many reasons someone may have low blood sodium levels, they are often more reflective of fluid status than dietary intake. Low sodium levels (less than 135 mEq/L) can indicate fluid overload, which is common when the kidneys are damaged due to impaired fluid excretion. High sodium levels (over 145 mEq/L) may suggest dehydration. It is a fine balance between the two, which is why it’s important to monitor sodium levels more closely during routine blood work.
Even without lab work, you can get a good indication of hydration through the color of your urine. Ideally, your urine should be the color of very light lemonade. If it’s too dark, it’s usually a good indicator to increase water intake. If it’s completely clear, ask your provider or dietitian about how to add more electrolytes to your daily routine.
Be Aware
If you have been diagnosed with late-stage kidney disease, you should ask your doctor if specific medications or supplements are safe to take.
Hope
Chronic kidney disease (CKD) used to be viewed as something that could not be reversed, but new research is offering hope. Studies are showing that certain changes can help improve kidney function and slow the progression of the disease. Eating a diet low in salt, phosphorus, and potassium, while adding more omega-3 fatty acids and antioxidants, can help reduce stress on the kidneys and improve blood pressure. New medications that target specific aspects of kidney damage are also showing promise. Scientists are even exploring stem cell therapy to repair damaged kidney tissue. While completely reversing CKD remains a challenge, these treatments, along with healthy habits like regular physical activity, proper nutrition, medical intervention, and quitting smoking, can make a significant difference in maintaining kidney health and slowing disease progression.
Sending Health Your Way!
The Tula Clinical Team
Reviewed by:
Aubree RN, BSN
Austin MS, RDN, CSR, LDN, CD
Tula Takeaways |
|---|
| 1. Diabetes and Kidney Health: These two are closely related, and it is important to monitor and know your baseline labs for both. Next time you visit your doctor, ask them for your BUN, creatinine, eGFR, potassium, and sodium levels. |
| 2. Keeping Your Values within Range: Work with your healthcare team to implement a care plan that helps improve values that may be out of range and keeps those within range stable. This might include simple actions like taking a walk each day or increasing your servings of fruits and vegetables to at least five per day to help manage your blood pressure. |
| 3. Caution around Supplements: It is always important to review your list of medications and supplements with your pharmacist, provider, and dietitian. |
The LIVE TULA blog is informational and not medical advice. Always consult your doctor for health concerns. LIVE TULA doesn’t endorse specific tests, products, or procedures. Use the information at your own risk and check the last update date. Consult your healthcare provider for personalized advice.






